Poster Title: Utilizing Nurse Navigation for Outpatient Mastectomies with or without Reconstruction
Organization or Hospital: John Muir Health
Authors: Sheila Marquez, RN, MSN, CBCN; Shellie Campos, RN, MSN, FNP-BC, AGN-BC; & Monica Eigelberger, MD, FACS
Conference Name: The Organization of Nurse Leaders of New Jersey ONLNJ Annual Meeting and Conference 2024
Presentation Date: May 05, 2022

Project Summary:
Historically, patients undergoing mastectomy surgeries at John Muir Health (JMH) required a one-night admission for postoperative care, pain management, and education support. However, research studies show that implementing Enhanced Recovery After Surgery (ERAS) pathways and patient education:
• improves outcomes
• improves patient satisfaction
• reduces hospital stay
JMH Nurse Navigator, Nurse Practitioner, and Breast Surgeon aimed to utilize ERAS pathways and patient education for patients undergoing a mastectomy to improving postoperative recovery and decreasing length of stay, patients’ fears, and anxieties.
This quality improvement project aims to decrease the length of stay for patients undergoing a mastectomy by utilizing nurse navigation patient education.
Methods:
The multidisciplinary team created a plan to implement ERAS pathways for mastectomy patients to decrease the length of stay. The Nurse Navigator developed the program by following our surgeon through a clinic day, surgery, and conducting a direct patient observation during a surgical day to understand the patient care flow. The Nurse Navigator created education sheets in both English and Spanish. In addition, provided a 1:1 in-person or virtual education focusing on:
• preoperative and postoperative instructions
• patient care flow
• postoperative exercises
• care of the drain
• instructions when to contact the surgeon postoperatively
Results:
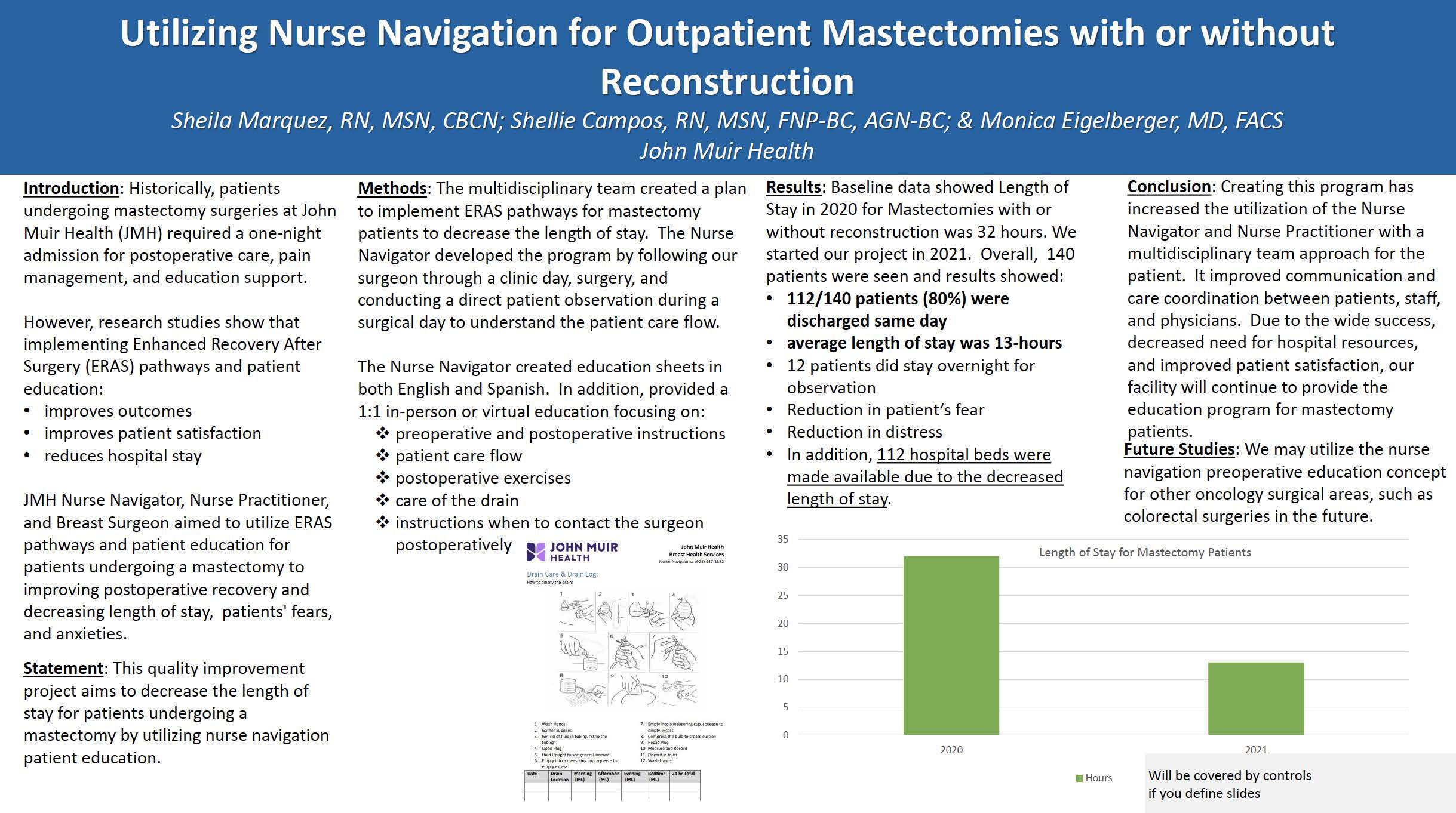
Results: Baseline data showed Length of Stay in 2020 for Mastectomies with or without reconstruction was 32 hours. We started our project in 2021. Overall, 140 patients were seen, and results showed:
• 112/140 patients (80%) were discharged same day.
• average length of stay was 13-hours.
• 12 patients did stay overnight for observation.
• Reduction in patient’s fear
• Reduction in distress
• In addition, 112 hospital beds were made available due to the decreased length of stay.
Conclusion:
Creating this program has increased the utilization of the Nurse Navigator and Nurse Practitioner with a multidisciplinary team approach for the patient. It improved communication and care coordination between patients, staff, and physicians. Due to the wide success, decreased need for hospital resources, and improved patient satisfaction, our facility will continue to provide the education program for mastectomy patients.
Future Studies: We may utilize the nurse navigation preoperative education concept for other oncology surgical areas, such as colorectal surgeries in the future.
Contact Person(s):
Tipton Health